Trust, Timing, and Technology: Understanding User Adoption in Adult Social Care

Adopting new technology is rarely just about the tech itself – it’s about relationships, confidence, and introducing the right support at the right moment.
Over the past year, we’ve been testing out different kinds of care technology in Redbridge, from digital health coaches to fall sensors, and learning a huge amount about what really works (and what doesn’t). Along the way, we’ve been sharing our reflections in this blog series, not just the polished successes but also the messy realities and surprises.
In this post, we’re zooming in on “user adoption”: what happens when someone is first introduced to a new piece of tech, how they get used to it (or don’t), and the role of trust, family, and everyday life in shaping whether it becomes part of their routine.
When you set out on a new pilot, it’s natural to plan for the “what ifs”, doing your due diligence, anticipating challenges, and making the best assumptions you can. But blind spots are inevitable. Some things only become clear once real people start using the technology, and that’s when the most valuable insights often emerge. What follows are some of the lessons we didn’t see coming and how they’re shaping our thinking for the future.
First encounters
With our pilot being focused on older adults of 60+ years, we have heard many concerns and feelings of caution around integrating technology into their care. Many people find it hard to keep up with the advances in modern technology, don’t understand how it works, worry that it might feel too intrusive and, as a result, do not show a lot of interest initially.
Some people however, become more curious after they have a conversation with a staff member who tells them about the potential benefits of care technology and gives them a demonstration of how it would work.
The single biggest influence in encouraging older adults to try care technology has been the support of close friends and family. For them, these tools often bring reassurance, offering a way to keep an eye on loved ones remotely and receive alerts if something seems wrong. Time and again, we’ve seen family members play a vital role in giving encouragement and explaining, in relatable terms, how care technology could make a real difference in their loved one’s life.
A few things we’ve found matter when introducing care technology to older adults:
- Keep it simple and hands-on. Explanations need to be clear, relatable, and supported by a demonstration. Leaflets can help, but only if written in accessible language and paired with a personal conversation.
- Tailor it to personal circumstances. People are more likely to see the value when the technology is linked to their own experiences. For example, after Mister X had a serious fall at night and couldn’t call for help, he understood how a fall sensor could alert his family straight away and prevent hours of waiting in pain.
- Frame it positively. Words matter: terms like “monitoring” or “tracking” can sound intrusive or threatening while talking about how technology can support independence and safety can feel more empowering.
Care tech supporting people in the right ways
Early findings from our evaluation of the pilot show that care technology can have a number of potential benefits for individuals:
- Residents experience some level of reassurance, knowing that technology gives those caring for them another ‘set of eyes’ in case something happens when they are alone (such as a fall), or because it might help to identify an emerging health issue earlier than would otherwise be the case. This reassurance is also experienced by close family members.
- Technology which provides residents with support to manage daily routines, such as appointment reminders and advice on activities to do (tailored to the individual’s interests and abilities) can also help to reduce anxiety, and promote independence and recovery from illness or injury.
- Staff in care settings find that care technology which monitors people’s movements and usual behaviours (especially overnight) can directly enable better quality, more tailored and more dignified care for their residents.
Care technology – the right fit for everyone?
Not every piece of care technology landed well in our pilot. Devices placed around the home or mounted on walls were often switched off or unplugged, while wearables were easily misplaced. These challenges were especially common among people living with memory loss or confusion, who couldn’t always remember why a new device had appeared in their space. “Do not touch” labels and plug covers helped a little, but ideally, the technology should be discreet, placed out of reach, or designed to blend naturally into everyday life.
One of our colleagues summed it up perfectly:
“Care technology shouldn’t just be made for people who are able to remember and follow instructions, such as keeping devices plugged in at all times. Care technology should be designed to accommodate people’s needs and experiences, not the other way round.”
This principle also applies to accessibility needs. While our pilot wasn’t focused on people with specific health conditions, one participant with hearing loss quickly highlighted the limits of certain devices that relied on verbal communication. It was a useful reminder that accessible options designed for a wide range of needs and abilities must always be part of any care technology offer.
Ultimately, there can be no one-size-fits-all approach. Care technology works best when it’s tailored to individual circumstances and flexible enough to adapt as those circumstances change.
Reaching those most in need of care tech
One of our biggest questions has been how to reach people at highest risk – those who could benefit most from care technology. We worked closely with the Redbridge Reablement Team, which sees up to 1,000 patients each year, and seemed a natural route to introduce tech that people could trial at home during (and beyond) their reablement journey.
In practice, uptake was slower than expected but not through the lack of trying. The team had leaflets, training and plenty of conversations with patients, yet many devices remained unused. Part of the challenge is that the criteria for participation were quite narrow and participation was voluntary. This meant that sometimes, those who we thought would benefit most, may not have been keen on the care tech. Once more, this highlights the importance of understanding a person’s unique circumstances and bringing out the selling points most relevant to their personal situation. We also suspect that people in reablement, often recovering from illness or injury, may be too focused on their health and immediate recovery to want to experiment with new technology at the same time.
By contrast, care homes and extra care facilities had the advantage that staff had existing, trusted relationships with residents, which made them more open to trying something new.
People’s willingness to adopt care technology is linked not only to how it’s explained, but also to their health, stability and life circumstances. Difficult or stressful periods may not be the right moment to introduce something new. An important lesson for us and a motivator to keep looking for better ways to ensure care technology reaches the right people, at the right time.
In summary – trust and timing matter:
- People are more open when technology is introduced by someone they know and trust and uptake is often higher in care settings where staff have long-standing relationships.
- Recovery or crisis periods aren’t always the right moment because high-pressure situations can limit willingness to try something new.
Care technology as an all-encompassing solution
We’ve also spent time reflecting on the risk of viewing care technology as an all-in-one solution. When that happens, there’s a danger that people lean on it too heavily, overlooking the need for human support and other forms of care.
At a recent event, we asked the audience what unintended consequences they could think of from the perspective of someone using care technology and this is what they said:
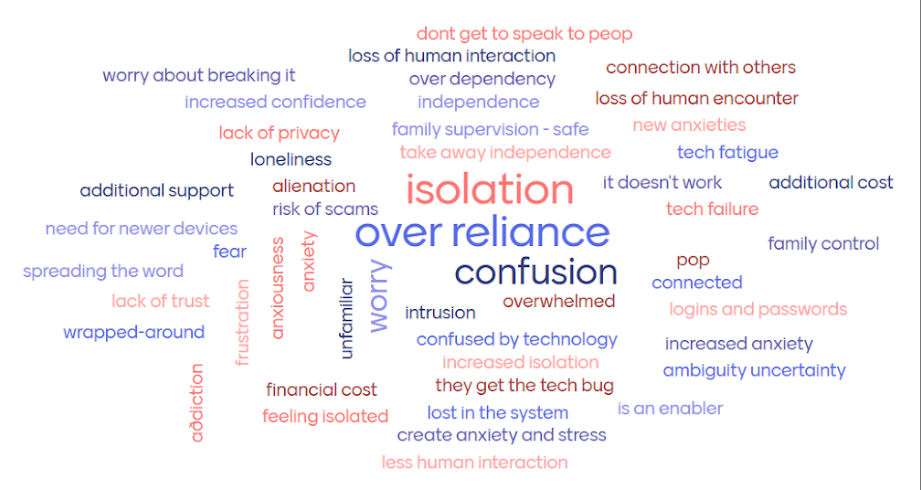
Isolation, over-reliance and confusion stand out from the word-cloud which reinforces our thesis that care technology defeats its purpose if:
- the use of care technology results in tying people to their home because they don’t feel comfortable leaving their house anymore
- loved ones or care teams neglect their duty of care because they rely solely on the data insights from an app or a dashboard, which results in the person using the care tech being much more isolated
- the care recipient feels confused and unsettled by a new device that has been installed in their house because they do not fully understand how it works
The key, we feel, is treating care technology as one of many tools in a toolbox. So it is critical to think about ways that care technology can successfully be integrated into someone’s life and how it can empower them to actively participate in their community, and reconnect with any activities that improve their wellbeing.
Final Thoughts
Care technology has huge potential, but the key is in how it’s introduced and supported. Our insights have shown that it works best when:
- It’s embedded alongside other forms of support, not as a standalone solution.
- It’s person-centred.
- It’s matched to someone’s individual goals and abilities.



