Reassurance and Realities: A Reablement Team’s Experience with Care Technology

NELFT‘s Reablement team shares what it’s really like to introduce care technology into short-term support, the practical challenges, the lessons learned, and the reassurance it brought to families.
Photo from L to R: Keelie Greaves & Amy Miller (Reablement), Cassandra Christie (Extra Care), Mags Kalaugher (Programme Manager), Emma Horgan & Jo Lincoln (Extra Care)
As part of the Redbridge Adult Social Care Tech Pilot, teams across the borough have been testing different care technologies to understand how they can support both residents and staff.
In this interview, we hear from the Reablement team, who share their experiences of introducing technology into short-term support, what worked, what was challenging, and most importantly, what they learned along the way.
Learning through doing
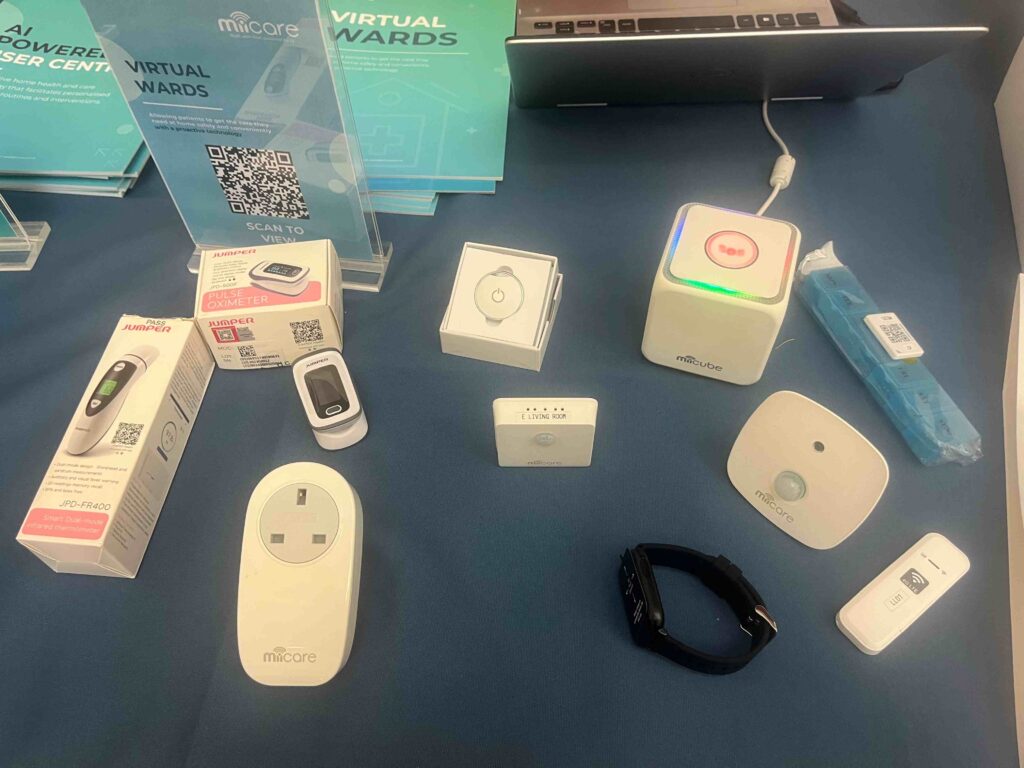
The Reablement service supports people who’ve recently left hospital or experienced a change in their health, helping them regain confidence and independence at home. For the pilot, the team introduced MiiCare, a digital health platform with motion sensors and a conversational device designed to monitor wellbeing and provide companionship.
Although the technology wasn’t directly integrated into the team’s day-to-day delivery because monitoring was handled by family members, the Reablement staff saw the pilot as a valuable learning opportunity.
Q: How have you found introducing MiiCare to your patients in the Reablement service?
Our role in Reablement was mainly to introduce patients and families to the technology and install it in their homes. From there, the monitoring was done by family members. Because our service is short-term, we are not in a position to do ongoing monitoring but it was really helpful to see how families engaged with it.
Overall, we’ve enjoyed getting to know MiiCare: seeing what it can do, how it works in practice, and what might make it more effective in the future. Families were generally very receptive to the technology, it seemed to give them a lot of reassurance and peace of mind, knowing they could see how their loved one was doing.
“It gave families a lot of reassurance and peace of mind.”
Some people also told us they really enjoyed the interactive element with Monica, the voice-activated digital companion. That companionship aspect was lovely to see.

Q: Can you tell us about the process of identifying clients to participate in this pilot?
One of our key learnings has been about timing. We found that the best time to identify clients for this kind of technology is while people are still in hospital and are being referred to Reablement. That early identification really helps.
We also learned a lot about the importance of matching the right technology to the right person. The criteria for who could receive MiiCare were quite specific, people needed to live alone, have English as their first language, and not have pets. We avoided offering it to anyone who might be confused or have early onset dementia, as we wanted to make sure it would be a positive experience for them.
There were a few unexpected moments too, like one patient who had the same name as the technology, which meant every time someone spoke to her, the device would respond!
Some patients already had smart devices like Alexa, so we learned that understanding what people already have at home is important before introducing something new.
And while some patients were a bit hesitant about electricity use or having technology in their homes, others were curious and open-minded once we explained the potential benefits.
Q: How did you find the experience of installing the MiiCare devices in people’s homes?
Installation was definitely a learning curve for us but we were able to build confidence over time. The training was good, but in practice, getting the sensors in the right places and connecting the cube to the internet was tricky at first. It often took a few attempts, and some installations lasted close to two hours.
Having hands-on support during the first few installations would have made a big difference just to make sure we were doing it right and to build confidence early on. The MiiCare team was really responsive with phone support, which helped a lot.
Over time, one team member became something of a “tech champion,” leading installations and helping others troubleshoot. In an ideal world, we’d all be able to carry out installations without having to rely on one team member.
There were also a few logistical challenges, like not being able to install the app on our work phones and having to use personal devices, or not always having all the contact details we needed to set up accounts. These were all valuable learnings for how to plan better next time.
Q: Is there any advice you’d like to share with someone who’s just starting out with care technology?
Start small and build confidence. It helps to have a clear process; who’s installing, who’s monitoring, who’s supporting families; that is making sure that everyone feels equipped.
We also learned that less is more when it comes to paperwork. There were a lot of leaflets, forms and questionnaires to complete, and simplifying that would make it easier for everyone involved if this sort of technology is to be used more widely.
And most importantly, don’t underestimate how much reassurance technology can bring to families. Even small things like being able to check in and know someone’s okay make a real difference.
Reflections
The Reablement team’s experience shows that introducing technology in short-term, transitional care can be as much about learning and confidence-building as it is about data or devices. From identifying the right clients early to simplifying processes, these insights offer practical lessons for anyone exploring digital care tools.
When new technology is introduced, it’s normal for people to have mixed feelings at first. There’s often some uncertainty and frustration as everyone gets used to something unfamiliar. But over time, as staff start to understand how the system works and see the benefits, things settle down.
Thandanani Ncube, Manager Redbridge Reablement Service (RRS)
A lot of that progress comes from working together to solve problems as they come up. Looking back, I think having more time for hands-on training at the start would have helped — it would have made the whole process a bit smoother for everyone.
While there were challenges along the way, the pilot also revealed the human side of innovation, the comfort families felt, the curiosity of patients, and the sense of empowerment that comes from trying something new.
“It’s all part of learning how technology can complement care — not replace it.”
In next week’s blog, we will hear from the Extra Care teams, who trialled two types of technologies with residents in their schemes.



